Introduction
Breast cancer poses a large health care burden. More than 270,000 women are diagnosed with breast cancer every year in the United States alone, and more than 40,000 women will die from the disease over the same period.1 Advances in routine screening and curative treatment options have led to mean 5-year survival rates for localized and regional disease of 98.9% and 85.7%, respectively.1 Diagnosis at an early stage, often due to routine screening, represents one of the most important prognostic factors for survival.
Routine mammography screening in average-risk women 50 years and older has reduced the age-adjusted mortality rate from breast cancer by 34% just over the past 20 years.2,3 While there is consensus among national health organizations regarding the benefits of routine mammographic screening in women 50 years and older, screening recommendations for average-risk women aged between 40 and 49 years vary.
Differences in screening recommendations among national organizations largely reflect variations in assessment of the benefit-to-harm ratio of screening women aged between 40 and 49 years who are less likely to develop breast cancer, compared with older women. Women who do develop breast cancer in this age group, however, are more likely to develop more aggressive disease.4,5 Over the past decade, this has become an increasingly important topic of discussion as breast cancer shifts to a younger age of onset.1 In this review, we examine the risks and benefits of routine breast cancer screening starting at age 40 at the individual level, followed by an evaluation of the role of advanced imaging techniques in screening women on a population level.
Current Breast Cancer Screening Guidelines
National health organizations update breast cancer screening recommendations primarily using pivotal, large-scale, multi-institutional randomized controlled trials (RCTs).2,6-12 RCTs inform meta-analyses and/or systematic reviews by stakeholder organizations for guideline formation. Updates to these recommendations are presented as new and long-term follow-up data become available.
In 2009, the US Preventive Services Task Force (USPSTF) recommended biennial mammographic screening for women aged between 50 and 74 years and updated these recommendations in 2016.13,14 In women aged between 40 and 49 years, the decision of periodic screening is based on individual self-assessment and risk profile; however, the USPSTF recommends against routine screening for average-risk women in this age group. The 2003 American Cancer Society (ACS) guidelines, updated in 2015, strongly recommend routine mammography screening for average-risk women annually (when aged between 45 and 54 years) or every 2 years (when 55 years or older).15,16 Women aged between 40 and 44 years should have the opportunity to begin annual screening based on individual risk, but there is less certainty about the balance of benefits relative to harms in this age group. The American College of Radiology (ACR) recommendations, made in collaboration with the Society of Breast Imaging (SBI), were published in 2010 and updated in 2017,17,18 and they include additional information to cover gaps in the previously issued USPSTF and ACS guidelines. The ACR/SBI recommends annual screening for women 40 years and older. The ACR/SBI also recommend annual screening for high-risk women younger than 40 years. There is considerable agreement among ACR/SBI screening recommendations and those of the American Society of Breast Surgeons,19 the National Comprehensive Cancer Network (NCCN),20 and the National Consortium of Breast Centers.21
In contrast to the USPSTF’s process for making recommendations, the ACS and the ACR/SBI also incorporate large observational study designs, those that evaluate breast cancer mortality, into their method for creating guidelines; the latter organizations also use modeling and simulation studies to supplement pivotal trial data. Using such studies in addition to RCTs allows for better reflection of current practice and a more robust representation of patient demographics throughout the treatment landscape in the United States. ACR/SBI guidelines also outline additional benefits of screening when it begins for average-risk women at age 45 years: reduction in the use of chemotherapy, earlier detection of high-risk disease, less aggressive forms of surgery, and improvements in life-years gained.18
Risk Stratification and Existing Guidelines
The USPSTF, ACR/SBI, and ACS agree that women with a strong familial history of breast cancer and/or ovarian cancer or a prior personal history of chest radiation therapy, or who are carriers of mutated BRCA1 or BRCA2 genes, have a higher cumulative lifetime risk of developing breast cancer. Therefore, different screening recommendations are warranted.13-21 High-risk women may be offered mammographic screening at ages younger than 40 years, more frequent screening, and/or supplemental imaging, such as ultrasound and MRI.15 Among average-risk women, there is significant heterogeneity in further risk stratification used to define both the age of initiation and the frequency of screening, and age remains the primary variable in screening recommendations for women younger than 50 years.15
Benefits and Harms of Breast Cancer Screening for Younger Women
The consensus among national health organizations is that mammographic screening in average-risk women is overall beneficial in reducing breast cancer mortality.3 However, key differences exist among organizations related to (1) recommended age to initiate screening and (2) frequency of routine screening.
Benefits
Across all organizations, the primary benefit of breast cancer screening is a reduction in breast cancer–specific mortality as outlined in pivotal RCT data. Overall breast cancer mortality as reported in a pooled analysis in women aged between 35 and 85 years was reduced between 11% and 36% in women screened with mammography compared with those who were not screened.22 Estimates quoted by the ACR/SBI meta-analysis similarly show a 26% to 39% reduction in breast cancer mortality with mammographic screening in women aged between 40 and 74 years.23,24 When incorporating the ACS meta-analyses, the breast cancer mortality reduction was 22% for the ACS and ACR/SBI groups, in comparison with 15% in the USPSTF groups.25 The difference in overall mortality reduction can potentially be attributed to the larger pool of studies included in the ACS and ACR/SBI analyses that represents more recent practice not captured in core RCT data. While the benefits of screening in women aged between 40 and 49 years is commonly referenced between ACR/SBI and ACS, these societies diverge in their recommendations in terms of when screening should commence. This is primarily due to ACR/SBI’s choice to incorporate factors such as a particular risk-benefit model that prioritizes life-years gained, racial disparities, and the impact of advanced imaging technologies.
When stratifying by age groups, there is a clear benefit when screening women aged between 40 and 49 years, although the magnitude of this benefit appears less than that of screening women 50 years and older due to overall lower incidence. The age-adjusted mortality reduction in the pivotal RCTs is lower than those presented in updated, large observational studies. Data from meta-analyses of RCTs showed a 15% to 35% mortality reduction with up to 18 years of follow-up in women 40 to 49 years of age,26 compared with 26% to 48% in large observational studies.27 The Swedish Mammography Screening in Young Women cohort study showed a 29% reduction in breast cancer mortality with 16-year follow-up after recommendations for invitation to screen in this younger age group.28
Breast cancer screening in women starting at age 40 has the potential to reduce mortality significantly and to lead to longer potential life spans (a 42% to 47% increase in the number of life-years gained) relative to when women are screened between ages 50 and 74 years.18,29,30 RCT data may not fully capture additional benefits of screening in this group; to do so may necessitate the incorporation of more recent, observational studies.
Harms
The benefits of routinely screening average-risk women aged between 40 and 49 years must be balanced with the harms associated with screening women who experience a lower incidence of breast cancer.31
False positive (FP) mammographic screening examinations that result in women being subsequently recalled for additional imaging or biopsy—but are eventually found to not have cancer—represent the primary harm of screening women in this younger age group. The incidence rate of FP findings has been estimated to be as high as 7% to 12% among women aged 40 to 59 years.14,23 In comparison, women aged 40 to 49 years have higher FP rates than women aged 50 to 59 years, with an odds ratio of 1.25 (95% CI, 1.23-1.26) due to denser breast tissue that impacts mammographic imaging sensitivity.32-34 Overall, an inverse relationship exists between age and FP and biopsy rates per 1000 screening exams for women older than 40 years.14,31 Anywhere from 80.0% to 87.3% of women with FP findings, however, undergo only additional imaging and not biopsy.36,37 A large retrospective cohort study of more than 200,000 women aged 50 to 69 years showed a low cumulative 20-year risk of 20.0%, 4.1%, and 2.0% for FP results, subsequent invasive procedures, and subsequent core biopsies, respectively.38
An early systematic review showed that women in the United States older than 40 years with FP screening findings are more likely than women of the same age who do not get FP screening findings to report greater psychological distress, anxiety about breast cancer, and worry over perceived risk of future breast cancer.39 While these exams have not been shown to lead to generalized anxiety or depression, breast cancer–specific distress related to FP results can persist for up to 3 years post screening mammogram.40 Despite these findings, up to 98% of adults in a United States survey who said that they were recalled following FP cancer screening examinations were satisfied that they had undergone the subsequent recommended test.41
The larger-scale economic harms of FP screening mammograms may be substantial. Each subsequent examination following FP screening findings ranged from $134.80 USD for follow-up imaging to $1374.69 USD for more invasive testing; this equates to an additional $5.26 million USD per 1000 women screened.42,43 In a 2015 study examining US health care expenditure data of more than 700,000 women, an 11% annual FP rate among screened women aged 40 to 49 years was estimated to cost an additional $2.8 billion annually (range, $1.2-$5.0 billion).34 Because FP findings incur such large additional costs, the individual benefits of annual screening for women aged 40 to 49 years need to be carefully balanced with the higher economic costs.
Overdiagnosis refers to screen-detected breast cancer that would not have progressed to clinical presentation during an individual’s lifetime nor would it have caused that individual harm in the absence of screening. This is a potential harm of increasing breast cancer screening examinations based on age and screening frequency; however, data are sparse. Estimates of overdiagnosis range from 5% to 50%,16,44-45 requiring significant assumptions that may overinflate results.46 Significant uncertainty still surrounds the magnitude of risks related to overdiagnosis, and further evaluation of this risk is necessary before informing action.45 Transitioning the focus of future studies to preventing overtreatment rather than overdiagnosis may represent a more prudent way of addressing management of more indolent tumors.
Advances in Imaging Technology
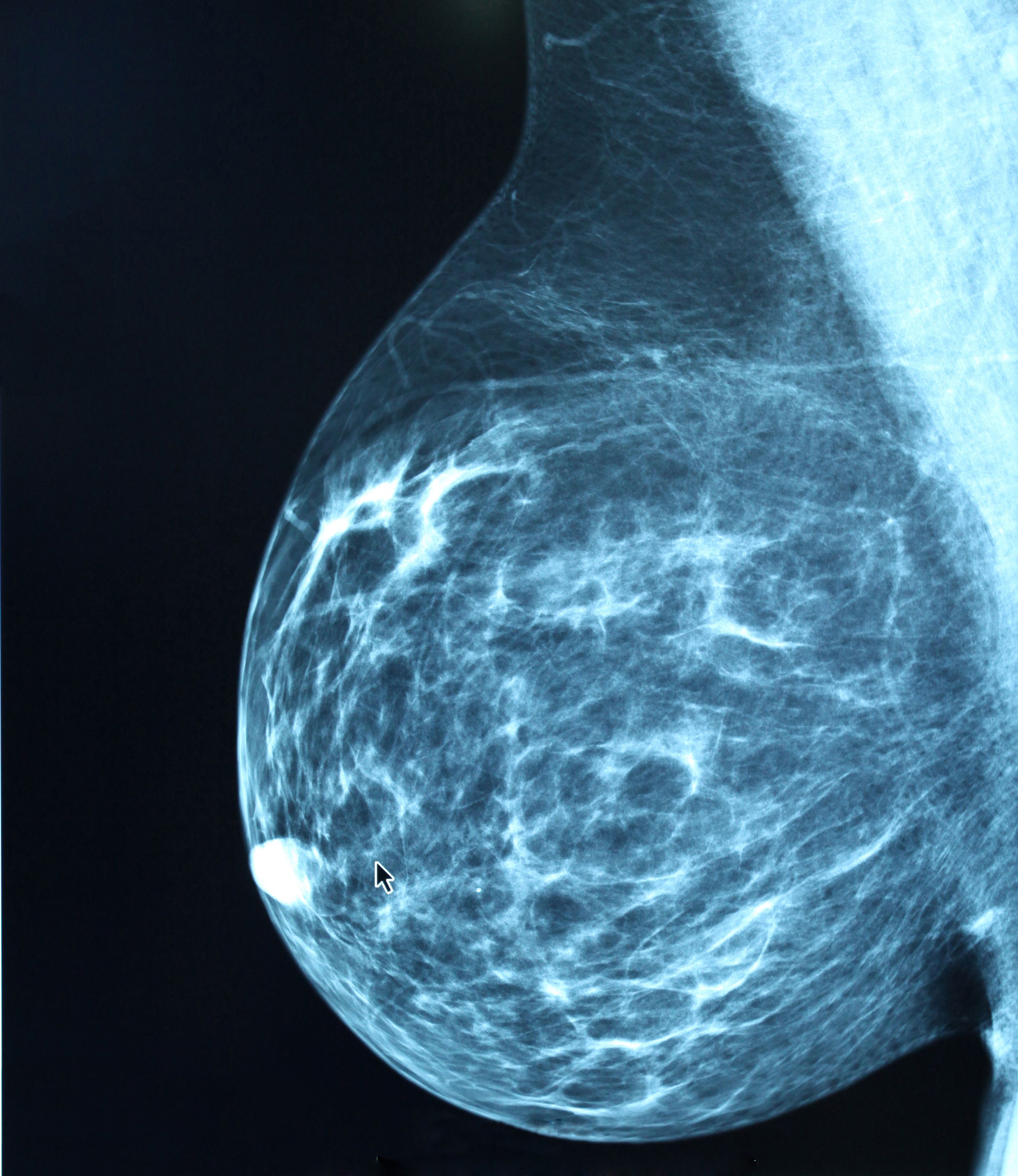
Mammography remains the gold standard for breast cancer screening but has well-established limitations. Use of advanced techniques purport improved cancer detection over full-field digital (2D) mammography alone. Appropriate use of advanced imaging technologies for screening may help maximize the overall benefit-to-harm ratio of screening average-risk women. We review these advanced imaging technologies here.47
Advances in Mammographic Imaging
Many of the pivotal RCTs informing guideline recommendations were completed with film-screen mammography. However, digital mammography is now widely used across the United States. The Digital Mammographic Imaging Screening Trial found no significant difference between film-screen and digital mammography in imaging sensitivity across more than 49,000 women in the United States and Canada.48 However, digital mammography had significant benefit over film-screen mammography when used in pre- and perimenopausal women, women younger than 50 years,49 and women with dense breasts.48
Digital breast tomosynthesis (DBT) or “3D” imaging is a recent advancement that demonstrates improved screening interpretation performance when combined with 2D digital mammography, compared with 2D digital mammography alone.49,50 Evidence is accumulating that shows recall rates and cancer detection are improved with the use of DBT.51-53 In a comparative effectiveness study in women aged 40 to 79 years, recall rates decreased from 24 of 1000 exams to 204 of 1000 exams, and cancer detection rates increased from 5.9 to 8.8 per 1000 exams.54
Contrast-enhanced screening mammography (CESM) provides the ability to identify angiogenesis induced by breast tumors. The examination involves a double exposure, using both low and high-energy x-rays. The result is a low-energy image, analogous to digital mammography, as well as recombined images demonstrating areas of enhancement with subtraction of background breast parenchyma, analogous to contrast-enhanced subtraction breast MRI images following contrast administration. CESM demonstrates improved diagnostic performance characteristics compared with digital mammography alone with better lesion detection and improved sensitivity and specificity.55 As practice evolves and advanced mammographic techniques become widely available, these techniques can be used to overcome limitations of 2D digital mammography.
Screening Breast Ultrasound
Screening breast ultrasound has shown additional benefits, particularly in women who have dense breast tissue that may obscure tumors on mammography. Incremental cancer detection rates of nearly 4.5 per 1000 women have been reported.56,57 Whole-breast ultrasound demonstrates a higher additional breast cancer detection rate than DBT, but increased FP examination rates associated with its use are not insignificant. High FP and biopsy rates as high as 8.8% have been reported.58 In addition, whole-breast ultrasound is largely a time-consuming, operator-dependent examination requiring technical expertise, which may limit utilization.
Breast MRI
Compared with digital mammography alone, supplemental breast MRI screening has been shown to increase diagnostic yield of small, node-negative tumors. Currently, it is the most sensitive supplemental screening technique, with an additional cancer detection rate of 15.5 per 1000 women screened. In addition, it has been shown to reduce interval cancer rates.59 While the ACS recommends an annual breast MRI in women with a lifetime risk of breast cancer that is greater than 20%,60-62 other women, including those with dense breasts and those at intermediate risk, may benefit from this technology. However, MRI screening is not routinely recommended for patients with average risk due to the increased risk of FP results and increased costs.63 In women who may derive benefit from breast MRI but who are not considered high risk, a viable option may be abbreviated breast MRI, which has been associated with shortened imaging time and decreased costs, offering the potential to widen its availability to more patients. Overall, abbreviated breast MRI has been shown to achieve a cancer detection rate similar to that of full multiparametric MRI protocols without sacrificing diagnostic accuracy.64,65
Conclusions and Future Directions
While national organizations differ in their recommendations related to initiation age and frequency of screening, there is consensus that, overall, routine mammography screening is beneficial in reducing breast cancer–specific mortality for average-risk women. While national organizations have not yet reached consensus about screening in younger women, improvement in advanced imaging techniques will, clearly, further support efforts to increase the benefit-to-harm ratio of routine mammographic screening in women younger than 50 years. Technological advances, including those in artificial intelligence, may eventually improve risk stratification and further
refine recommendations. Risk-based screening using more accurate tools appears to represent a viable solution for health care providers to determine which women require earlier and more frequent screening; these tools can also contribute to reducing the anxiety and FP results often associated with increased screening frequency in women at low risk.
Recently, the USPSTF published a draft research plan to be used to update their breast cancer screening recommendations; it will include study designs in addition to RCTs. The evaluation of racial disparities on breast cancer screening and outcomes will also be included in the updated USPSTF plan and marks an important step in consideration of additional risk factors in future screening recommendations.66 This may be an indicator of eventual convergence of national screening recommendations; however, collaboration among stakeholders, with continued reassessment of data, will be needed to achieve true consensus among organizations. In turn, this will lead to improvements in clinical management of preventive care as well as reductions in patient confusion related to breast cancer screening.
Financial Disclosure: RCM receives grant funding from General Electric through the AUR GERRAF Fellowship Award. AN works at MOLLI Surgical. AR works at MOLLI Surgical.
References
- SEER data, 1975-2018. National Cancer Institute/Surveillance, Epidemiology, and End Results Program. Updated August 1, 2019. Accessed March 1, 2021. https://ift.tt/3gJK6sp
- Shapiro S, Venet W, Strax P, Venet L, Roeser R. Ten- to fourteen-year effect of screening on breast cancer mortality. J Natl Cancer Inst. 1982;69(2):349-355.
- Narayan AK, Lehman CD. Mammography screening guideline controversies: opportunities to improve patient engagement in screening. J Am Coll Radiol. 2020;17(5):633-636. doi:10.1016/j.jacr.2020.01.001
- Fletcher SW. Breast cancer screening among women in their forties: an overview of the issues. J Natl Cancer Inst Monogr. 1997;(22):5-9. doi:10.1093/jncimono/1997.22.5
- Sox HC. Screening mammography in women younger than 50 years of age. Ann Inter Med. 1995;122(7):550-552. doi:10.7326/0003-4819-122-7-199504010-00013
- Miller AB, Baines CJ, To T, Wall C. Canadian National Breast Screening Study: 1. breast cancer detection and death rates among women aged 40 to 49 years. CMAJ. 1992;147(10):1459-1476.
- Miller AB, To T, Baines CJ, Wall C. The Canadian National Breast Screening Study-1: breast cancer mortality after 11 to 16 years of follow-up. a randomized screening trial of mammography in women age 40 to 49 years. Ann Intern Med. 2002;137(5 Pt 1):305-312. doi:10.7326/0003-4819-137-5_part_1-200209030-00005
- Moss SM, Cuckle H, Evans A, et al. Effect of mammographic screening from age 40 years on breast cancer mortality at 10 years’ follow-up: a randomised controlled trial. Lancet. 2006;368(9552):2053-2060. doi:10.1016/S0140-6736(06)69834-6
- Frisell J, Lidbrink E, Hellstrom L, Rutqvist LE. Followup after 11 years—update of mortality results in the Stockholm mammographic screening trial. Breast Cancer Res Treat. 1997;45(3):263-270. doi:10.1023/a:1005872617944
- Andersson I, Aspegren K, Janzon L, et al. Mammographic screening and mortality from breast cancer: the Malmö mammographic screening trial. BMJ. 1988;297(6654):943-948. doi:10.1136/bmj.297.6654.943
- Bjurstam N, Björneld L, Warwick J, et al. The Gothenburg Breast Screening Trial. Cancer. 2003;97(10): 2387-2396. doi:10.1002/cncr.11361
- Tabar L, Fagerberg G, Chen HH, et al. Efficacy of breast cancer screening by age. new results from the Swedish Two-County Trial. Cancer. 1995;75(10):2507-2517. doi:10.1002/1097-0142(19950515)75:10<2507::aid-cncr2820751017>3.0.co;2-h
- US Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(10):716-726, W-236. doi:10.7326/0003-4819-151-10-200911170-00008
- Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2016;164(4):244-255. doi:10.7326/M15-0969
- Smith RA, Saslow D, Andrews Sawyer K, et al; American Cancer Society High-Risk Work Group; American Cancer Society Screening Older Women Work Group; American Cancer Society Mammography Work Group; American Cancer Society Physical Examination Work Group; American Cancer Society New Technologies Work Group; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53(3):141-169. doi:10.3322/canjclin.53.3.141
- Oeffinger KC, Fontham ETH, Etzioni R, et al; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599-1614. doi:10.1001/jama.2015.12783
- Lee CH, Dershaw DD, Kopans D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18-27. doi:10.1016/j.jacr.2009.09.022
- Monticciolo DL, Newell MS, Hendrick RE, et al. Breast cancer screening for average-risk women: recommendations from the ACR Commission on Breast Imaging. J Am Coll Radiol. 2017;14(9):1137-1143. doi:10.1016/j.jacr.2017.06.001
- Position statement on screening mammography. American Society of Breast Surgeons. Updated May 3, 2019. Accessed April 12, 2021. https://ift.tt/3gGYAYFf
- NCCN. Clinical Practice Guidelines in Oncology. Breast cancer screening and diagnosis, version 5.2020. Accessed April 12, 2021. https://ift.tt/3vEpO7C
- National Consortium of Breast Centers, Inc. position statement regarding the mammography screening recommendations of the United States Preventive Services Task Force (USPSTF). National Consortium of Breast Centers. Updated March 16, 2018. Accessed April 12, 2021. https://ift.tt/3gCraeJ
- Broeders M, Moss S, Nyström L, et al; EUROSCREEN Working Group. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(Suppl 1):14-25. doi:10.1258/jms.2012.012078
- Kerlikowske K, Grady D, Rubin SM, Sandrock C, Ernster VL. Efficacy of screening mammography. a meta-analysis. JAMA. 1995;273(2):149-154.
- Duffy SW, Tabár L, Chen H-H, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95(3):458-469. doi:10.1002/cncr.10765
- Tabár L, Vitak B, Chen TH, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011;260(3):658-663. doi:10.1148/radiol.11110469
- Hendrick RE, Smith RA, Rutledge JH 3rd, Smart CR. Benefit of screening mammography in women aged 40-49: a new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;(22):87-92. doi:10.1093/jncimono/1997.22.87
- Andersson I, Janzon L. Reduced breast cancer mortality in women under age 50: updated results from the Malmö Mammographic Screening Program. J Natl Cancer Inst Monogr. 1997;(22):63-67. doi:10.1093/jncimono/1997.22.63
- Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer. 2011;117(4):714-722. doi:10.1002/cncr.25650
- Expert Panel on Breast Imaging; Mainiero MB, Moy L, Baron P, et al. ACR Appropriateness Criteria breast cancer screening. J Am Coll Radiol. 2017;14(11S):S383-S390. doi:10.1016/j.jacr.2016.09.021
- Hendrick RE, Helvie MA, Hardesty LA. Implications of CISNET modeling on number needed to screen and mortality reduction with digital mammography in women 40-49 years old. AJR Am J Roentgenol. 2014;203(6):1379-1381.doi:10.2214/AJR.14.12646
- Siu AL; U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164(4):279-296. doi:10.7326/M15-2886
- Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998;338(16):1089-1096. doi:10.1056/NEJM199804163381601
- Armstrong K, Moye E, Williams S, Berlin JA, Reynolds EE. Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians. Ann Intern Med. 2007;146(7):516-526. doi:10.7326/0003-4819-146-7-200704030-00008
- Ong M-S, Mandl KD. National expenditure for false-positive mammograms and breast cancer overdiagnoses estimated at $4 billion a year. Health Aff (Millwood). 2015;34(4):576-583.doi:10.1377/hlthaff.2014.1087
- Nelson HD, Cantor A, Humphrey L, et al. Screening for Breast Cancer: A Systematic Review to Update the US Preventive Services Task Force Recommendation. Agency for Healthcare Research and Quality (US); 2016.
- Canadian Partnership Against Cancer (CPAC). Breast cancer screening in Canada: monitoring and evaluation of quality indicators—results report 2011 to 2012 (2017). CPAC. 2017. Accessed April 12, 2021. https://ift.tt/3vGYyW9
- Chubak J, Boudreau DM, Fishman PA, Elmore JG. Cost of breast-related care in the year following false positive screening mammograms. Med Care. 2010;48(9):815-820.doi:10.1097/MLR.0b013e3181e57918
- Roman M, Hubbard RA, Sebuodegard S, Miglioretti DL, Castells X, Hofvind S. The cumulative risk of false-positive results in the Norwegian Breast Cancer Screening Program: updated results. Cancer. 2013;119(22):3952-3958. doi:10.1002/cncr.28320
- Brewer NT, Salz T, Lillie SE. Systemic review: the long-term effects of false-positive screening mammograms. Ann Intern Med. 2007;146(7):502-510. doi:10.7326/0003-4819-146-7-200704030-00006
- Bond M, Pavey T, Welch K, et al. Systematic review of the psychological consequences of false-positive screening mammograms. Health Technol Assess. 2013;17(13):1-170, v-vi. doi:10.3310/hta17130
- Schwartz LM, Woloshin S, Fowler FJ Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71-78. doi:10.1001/jama.291.1.71
- Stout NK, Lee SJ, Schechter CB, et al. Benefits, harms, and costs for breast cancer screening after US implementation of digital mammography. J Natl Cancer Inst. 2014;106(6):dju092. doi:10.1093/jnci/dju092
- Paci E, Miccinesi G, Puliti D, et al. Estimate of overdiagnosis of breast cancer due to mammography after adjustment for lead time. a service screening study in Italy. Breast Cancer Res. 2006;8(6):R68. doi:10.1186/bcr1625
- Puliti D, Duffy SW, Miccinesi G, et al; EUROSCREEN Working Group. Overdiagnosis in mammographic screening for breast cancer in Europe: a literature review. J Med Screen. 2012;19(Suppl 1):42-56. doi:10.1258/jms.2012.012082
- Jørgensen KJ, Gøtzsche PC. Overdiagnosis in publicly organized mammographic screening programmes: systemic review of incidence trends. BMJ. 2009:339:b2587. doi:10.1136/bmj.b2587
- Desreux JAC. Breast cancer screening in young women. Eur J Obstet Gynecol Reprod Biol. 2018;230:208-211. doi:10.1016/j.ejogrb.2018.05.018
- Pisano ED, Gatsonis C, Hendrick E, et al; Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast cancer screening. N Engl J Med. 2005;353(17):1773-1783. doi:10.1056/NEJMoa052911
- Pisano ED, Hendrick RE, Yaffe MJ, et al; DMIST Investigators Group. Diagnostic accuracy of digital versus film mammography: exploratory analysis of selected population subgroups in DMIST. Radiology. 2008;246(2):376-383. doi:10.1148/radiol.2461070200
- Conant EF, Barlow WE, Herschorn SD, et al; Population-based Research Optimizing Screening Through Personalized Regimen (PROSPR) Consortium. Association of digital breast tomosynthesis vs digital mammography with cancer detection and recall rates by age and breast density. JAMA Oncol. 2019;5(5):635-642. doi:10.1001/jamaoncol.2018.7078
- Ciatto S, Houssami N, Bernardi D, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study.Lancet Oncol. 2013;14(7):583-589. doi:10.1016/S1470-2045(13)70134-7
- Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311(24):2499-2507. doi:10.1007/s10549-016-3695-1
- Fujii MH, Herschorn SD, Sowden M, et al. Detection rates for benign and malignant diagnoses on breast cancer screening with digital breast tomosynthesis in a statewide mammography registry study.AJR Am J Roentgenol. 2019;212(3):706-711. doi:10.2214/AJR.18.20255
- Bernardi D, Macaskill P, Pellegrini M, et al. Breast cancer screening with tomosynthesis (3D mammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol. 2016;17(8):1105-1113. doi:10.1016/S1470-2045(16)30101-2
- Lowry KP, Coley RY, Miglioretti DL, et al. Screening performance of digital breast tomosynthesis vs digital mammography in community practice by patient age, screening round, and breast density. JAMA Netw Open. 2020;3(7):e2011792. doi:10.1001/jamanetworkopen.2020.11792
- Sung JS, Lebron L, Keating D, et al. Performance of dual-energy contrast-enhanced digital mammography for screening women at increased risk of breast cancer. Radiology. 2019;293(1):81-88. doi:10.1148/radiol.2019182660
- Crystal P, Strano SD, Shcharynski S, Koretz MJ. Using sonography to screen women with mammographically dense breasts. AJR Am J Roentgenol. 2003;181(1):177-182. doi:10.2214/ajr.181.1.1810177
- Berg WA, Blume JD, Cormack JB, et al; ACRIN 6666 Investigators. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008;299(18):2151-2163. doi:10.1001/jama.299.18.2151
- Gordon PB. Ultrasound for breast cancer screening and staging. Radiol Clin North Am. 2002;40(3):431-441. doi:10.1016/s0033-8389(01)00014-8
- Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology. 2017;283(2):361-370. doi:10.1148/radiol.2016161444
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75-89. doi:10.3322/canjclin.57.2.75
- Griebsch I, Brown J, Boggis C, et al; UK Magnetic Resonance Imaging in Breast Screening (MARIBS) Study Group. Cost-effectiveness of screening with contrast enhanced magnetic resonance imaging vs X-ray mammography of women at a high familial risk of breast cancer. Br J Cancer. 2006;95(7):801-810. doi:10.1038/sj.bjc.6603356
- Miles RC, Onega T, Lee CI. Addressing potential health disparities in the adoption of advanced breast imaging technologies. Acad Radiol. 2018;25(5):547-551. doi:10.1016/j.acra.2017.05.021
- Morrow M, Waters J, Morris E. MRI for breast cancer screening, diagnosis, and treatment. Lancet. 2011;378(9805):1804-1811. doi:10.1016/S0140-6736(11)61350-0
- Panigrahi B, Mullen L, Falomo E, Panigrahi B, Harvey S. An abbreviated protocol for high-risk screening breast magnetic resonance imaging: impact on performance metrics and BI-RADS assessment. Acad Radiol. 2017;24(9):1132-1138. doi:10.1016/j.acra.2017.03.014
- Dialani V, Tseng I, Slanetz PJ, et al. Potential role of abbreviated MRI for breast cancer screening in an academic medical center. Breast J. 2019;25(4):604-611. doi:10.1111/tbj.13297
- Palmer WJ. Industry experts applaud changes behind USPSTF breast screening guidelines update. January 27, 2021. Accessed April 12, 2021. https://ift.tt/3wHlG8a
"breast" - Google News
June 18, 2021 at 11:21PM
https://ift.tt/35AwAAN
Routine Breast Cancer Screening in Average-Risk Women Younger Than 50 Years: Current Paradigms Based on National Guidelines - Cancer Network
"breast" - Google News
https://ift.tt/2ImtPYC
https://ift.tt/2Wle22m
Bagikan Berita Ini














0 Response to "Routine Breast Cancer Screening in Average-Risk Women Younger Than 50 Years: Current Paradigms Based on National Guidelines - Cancer Network"
Post a Comment