For 19 years, Jennifer Gail has felt like her breasts are not her own.
Gail was diagnosed at age 36 with stage 4 (metastatic) breast cancer, which led to her first reconstructive surgery on her left breast. Some patients immediately have reconstructive surgery after their breast is removed, but her cancer’s location in a lymph node created an obstacle for that procedure.
For six months, it was too painful to look in the mirror at the space where her breast used to be.
Eventually, a breast surgeon inserted a tissue expander, which stretches the breast skin and muscle to create space for a permanent breast implant.
On HoustonChronicle.com: What is the BRCA gene and should you get tested for it?
“Reconstruction for me was part of moving forward and healing; getting your body and your life back,” said Gail, now 55. “It’s very traumatic for women to lose their breasts.”
Four years ago, she was diagnosed with stage 1 cancer in her right breast, which resulted in a flap procedure where fat and skin from her stomach was inserted in the area where her breast was.
Gail is grateful for her health, but admits she misses the way she looked in clothes before. She has little-to-no breast or nipple sensation. She feels her breasts are mismatched.
For decades, women who have recovered from breast cancer or had preventive surgeries have dealt with imperfect solutions for how their breasts look and feel after a mastectomy. The problem is more than aesthetic; mismatched breasts can lead to body insecurity and a feeling of being less feminine.
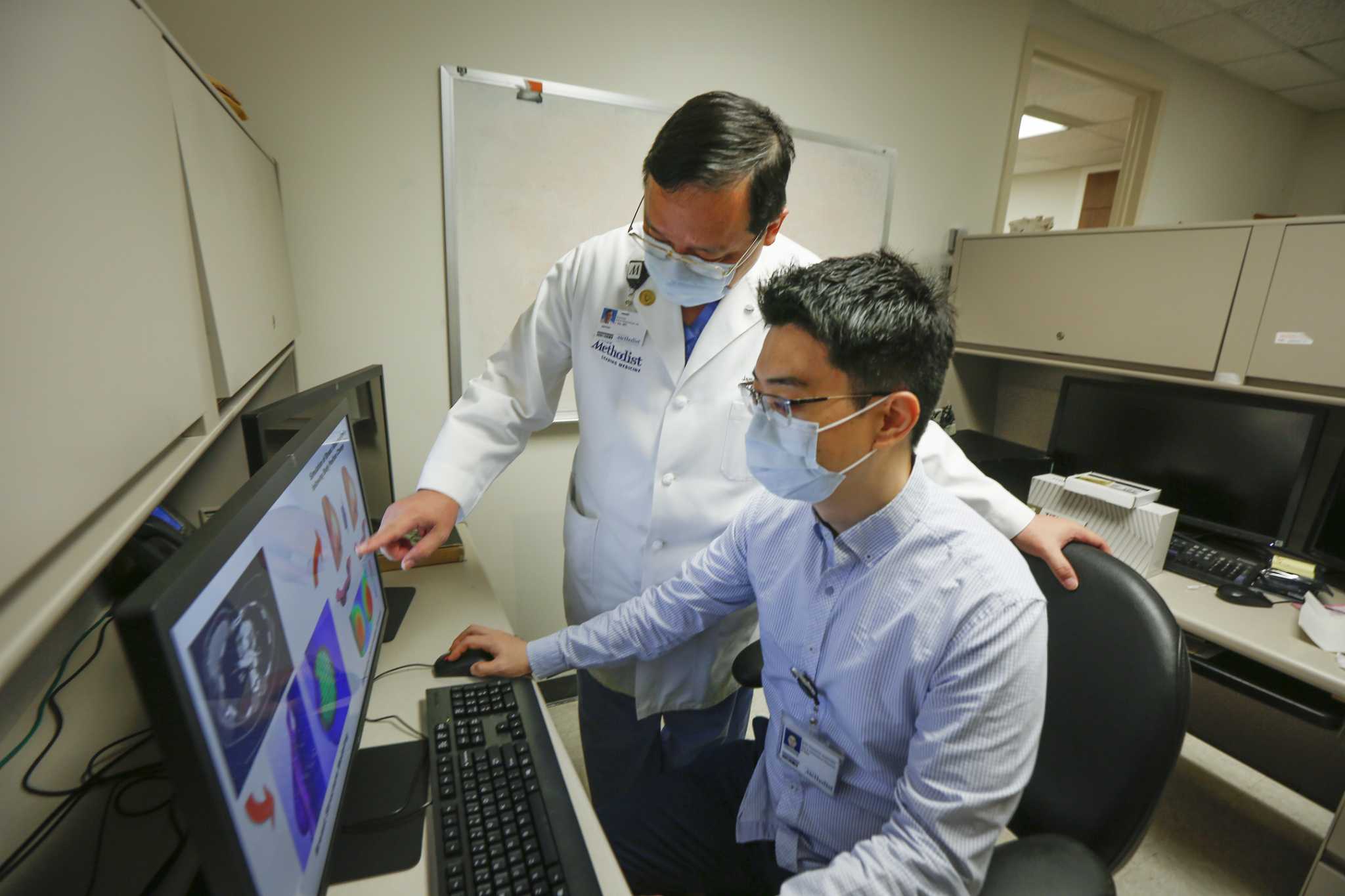
Now, Gail is one of four women taking part in a clinical trial that could lead to the first customizable breast implants for mastectomy and lumpectomy patients. The Houston Methodist trial is collecting marker-based computed tomography (CT) and 3D photo images of the upper body of breast cancer patients to create a computer-based model for personalized implants.
Off-the-shelf implants typically come in small, medium and large, said Dr. Jenny Chang, director of Houston Methodist Cancer Center and Gail’s oncologist. While reconstruction surgery has improved to spare the breast skin and areolas, there have not been major changes to permanent breast implants.
And there are complications with the department-store sizing model. Chang said it’s like buying a suit that only comes in three sizes and can’t be tailored, forcing you to buy one that is too big and use padding to fit. It doesn’t make sense, she said.
It’s not uncommon for patients to be dissatisfied with the results of their initial surgery and plan a second one on the healthy breast in the hopes of matching the size and shape of the newly implanted one.
“Often, they can’t match it to the good boob. What they do is give you a big one and put a little implant on the other side to match it,” Chang said. “Why would you need to touch the good side?”
On HoustonChronicle.com: Houston spa owner gives breast cancer survivors free areola tattoos
In mid-2019, Chang asked Dr. James Xia with the Houston Methodist Research Institute, to help find a solution to the mismatch problem. He has used 3D technology for facial and cranial reconstruction surgeries, but has little experience in breast surgery.
Soft tissue is much different than the bony structure of a face, he said. There are no supporting structures inside breasts, and they change depending on if the woman is in a supine or upright position, he said.
As he continues to study how tissue changes, James has developed a theory about the biomechanical properties of a breast shifting when the body changes position. Researchers believe 3D technology using breast scans from women with natural and reconstructed breasts will help them create a custom breast implant.
“We’re getting a lot of data and making great progress,” Chang said. “We want to give (women) a bespoke boob that matches their other breast. Big or small, the right size and consistency is the goal.”
And it’s been a long time coming.
The first mastectomy was performed in the 1880s; and the procedure continues to be the standard operation to treat or prevent breast cancer. But issues like breast sensation, correct sizing and aesthetics have only been researched for about 30 years, said Dr. Aldona Spiegel, a plastic reconstruction surgeon at Methodist.
The challenge has always been breast sensation restoration, she said.
On HoustonChronicle.com: Do I need a mammogram?
Newer surgery techniques, such as nipple-sparing and flap procedures, have improved aesthetic results by allowing for tissue placement above the pectoral muscle, which is considered a more natural location. The fat and skin is typically taken from the person’s stomach.
However, implant-based reconstruction involves the removal of all breast tissue, which means nerves are cut during the during the procedure. Loss of nerves means a loss of sensation, Spiegel said.
“The return of sensation is variable after a mastectomy. Some do have some sensation, but there are a group of patients who have very little sensation,” Spiegel said. “It’s obviously a problem for protective sensation (feeling a burn or sharp pain), but it’s a part of femininity.”
Recently, a cellular collagen graft was developed and is available for implant-based reconstruction patients, she said. During surgery, the nerve that is cut is then connected to the graft, which allows for more nerves to grow, eventually delivering sensation to the nipple and new breast skin.
The graft comes from a donor and is stripped of its cells until it is only made up of collagen, Spiegel said. Her first patient to request this technique was in 2018. The young woman was set to have a double mastectomy after testing positive for the BRCA1, or breast cancer, gene and worried about loss of sensation.
Renew Houston: Get the latest wellness news delivered to your inbox
“The decision to have an elective mastectomy is very difficult for patients who are young and in the prime of their life,” Spiegel said. “It’s important to determine with the patient their thoughts about their own breast sensation.”
The novel technique is not used in many plastic surgery centers yet, she added, because of the unpredictability of nerve regrowth and how long it could take. Sensation and nerve growth does improve over time.
Patients drive progress — especially when you listen to them, she said. The way breasts look and how they feel are two separate reasons why there continues to be research and advancement for breast implants for breast cancer patients.
Gail, who leads a Christian breast cancer support group at River Point Church in Missouri City, decided to join the customized implant clinical study to help others.
“It was founded on Proverbs 3:5: ‘Trust in the Lord with all your heart. And lean not on your own understanding,’” Gail said. “It’s about moving forward. That’s why I like to do studies; I want to give back and walk along other women.”
julie.garcia@chron.com
Twitter.com/reporterjulie
"breast" - Google News
October 28, 2020 at 10:00PM
https://ift.tt/34B8MNF
New breakthroughs in breast implants provide hope for breast cancer patients - Houston Chronicle
"breast" - Google News
https://ift.tt/2ImtPYC
https://ift.tt/2Wle22m
Bagikan Berita Ini














0 Response to "New breakthroughs in breast implants provide hope for breast cancer patients - Houston Chronicle"
Post a Comment