Breast cancer is now the most-diagnosed cancer worldwide. With 2.3 million new cases revealed in 2020, it’s not a problem that’s going away in any hurry. But researchers are looking at new ways to treat it – with some promising leads.
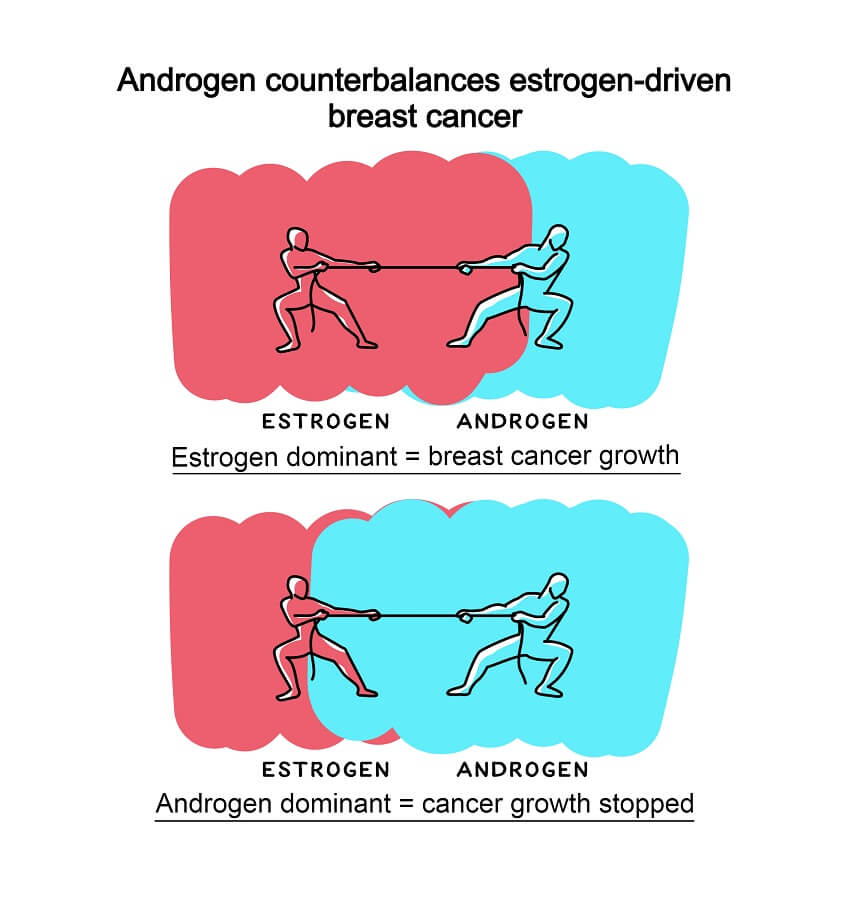
The crux of a lot of breast cancer treatment lies in hormones: specifically, in estrogens and androgens.
Androgens are usually thought of as “male” sex hormones – responsible for encouraging male secondary sex characteristics, such as facial hair and Adam’s apples. Estrogens are “female” hormones; they play a major role in breast development during puberty, among other things.
The two classes of hormone are similar on a molecular level. In fact, estrogens are actually made out of androgens in the human body – they’re created from androstenedione, which is an androgen itself, but is also used to make testosterone. The body’s enzymes convert it into other hormones depending on sex.
The vast majority of breast cancers are diagnosed in women, so it makes sense that estrogens would be the target for breast-cancer treatments.
“The large majority – at least 80% or more – of breast cancers are driven by the estrogen receptor [ER],” says breast cancer research specialist Theresa Hickey, an associate professor at the University of Adelaide. “For over 70 years, the main treatment strategy has been to completely wipe out ER activity using drugs collectively referred to as ‘endocrine therapy’.”
But it’s not as simple as a female/male divide when it comes to hormones. Women have some androgens as well, just has men have some estrogens.
“Men need estrogen too, they just have a dominant androgen environment,” says Hickey.
“Whereas in women, we produce those hormones, but we convert the large majority of it to estrogen hormones. So it was always thought that well, the little bits left can’t be functional. Surely the role of androgen hormones in a woman is to make estrogen hormones.
“Now we know that’s not true. A lot of androgen receptors are all over the female body, and that little bit of androgen hormone is very vital to women’s health.”
This is particularly relevant to breast cancer. While most breast-cancer treatments revolve around estrogen receptors, Hickey’s research team has published a paper that pursues an alternative strategy. Their research shows that androgen receptors can suppress tumours.
The data’s taken 10 years to collect, and it’s comprehensive. There is evidence from several different lines of inquiry – including studies on breast tissues, mice, and cell lines from patients.
“We were aiming not only to advance knowledge but provide compelling evidence to support a major change in patient care,” says Hickey.
“We investigated clinical breast cancers by looking at markers of the androgen receptor and its activity. And then we had developed a method of collecting tumours from surgery … and culturing them in the lab as slices and being able to treat them with drugs to see the response of the actual patient tumours. So that was another layer of evidence. And then we had the mouse models … they act almost as patient avatars.”
The research is “as close to treating the patient as you can get”.
Hickey says that androgen receptors have been suggested as possible targets for breast cancer treatment since the early 1990s, but this is the first comprehensive evidence in their favour.
And in fact, androgens were used in breast cancer treatment during the 1950s and ’60s. But their use wasn’t popular, because “people did not have a clue about why it worked and who best to give the therapy to”.
They also had a virilizing effect: they prompted male physical traits such as excess facial and body hair growth, deepening of the voice, and other effects that weren’t popular with women.
Fortunately, pharmaceutical science has also moved on since the 1960s.
“Newer generation drugs called selective androgen receptor modulators (SARMs) can have androgenic actions in the breast but do not have virilizing side effects,” says Hickey.
One in particular – Enobosarm – can even be beneficial for women. Developed initially to treat bone and muscle wasting in women and men with cancer, the drug is now in phase 3 trials for treating breast cancer in the US.
“They say women feel good on this drug,” says Hickey. That’s a sharp contrast to traditional, estrogen-focussed endocrine therapy treatments, which “have debilitating side effects” and can make women “feel absolutely miserable”.
“While endocrine therapies have prolonged life for many, it is not curative, and the major cause of breast-cancer death is disease that has become completely resistant to current endocrine therapies.”
The next step, according to Hickey, is to test these new androgen receptor drugs in patients – first alongside traditional treatments, and then hopefully on their own.
Things are changing quickly, in medical terms. The advantage of the Enosobarm treatment is that it’s been extensively tested in humans and so has been shown to be non-toxic and safe to take. “Those hoops have already been gone through,” says Hickey.
“If the trial succeeds, this therapy may be in the clinic within 2–3 years.”

Ellen Phiddian
Ellen Phiddian is a science journalist at The Royal Institution of Australia.
Read science facts, not fiction...
There’s never been a more important time to explain the facts, cherish evidence-based knowledge and to showcase the latest scientific, technological and engineering breakthroughs. Cosmos is published by The Royal Institution of Australia, a charity dedicated to connecting people with the world of science. Financial contributions, however big or small, help us provide access to trusted science information at a time when the world needs it most. Please support us by making a donation or purchasing a subscription today.
"breast" - Google News
March 08, 2021 at 03:02AM
https://ift.tt/3bryFTw
Exploring treatments in breast cancer - Cosmos
"breast" - Google News
https://ift.tt/2ImtPYC
https://ift.tt/2Wle22m
Bagikan Berita Ini














0 Response to "Exploring treatments in breast cancer - Cosmos"
Post a Comment