Abstract
Background
Receiving a breast cancer diagnosis can be a turning point with negative impacts on mental health, treatment and prognosis. This meta-analysis sought to determine the nature and prevalence of clinically significant psychological distress-related symptoms in the wake of a breast cancer diagnosis.
Methods
Ten databases were searched between March and August 2020. Thirty-nine quantitative studies were meta-analysed.
Results
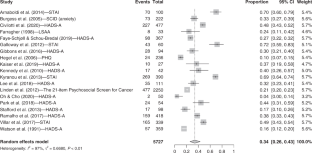
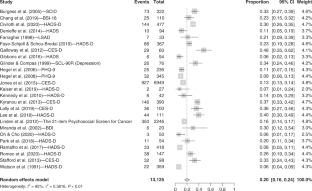
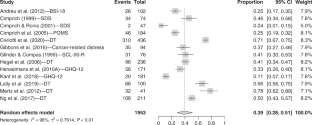
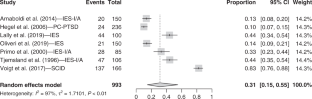
The prevalence of clinically significant symptoms was 39% for non-specific distress (n = 13), 34% for anxiety (n = 19), 31% for post-traumatic stress (n = 7) and 20% for depression (n = 25). No studies reporting breast cancer patients’ well-being in our specific time frame were found.
Conclusion
Mental health can be impacted in at least four domains following a diagnosis of breast cancer and such effects are commonplace. This study outlines a clear need for mitigating the impacts on mental health brought about by breast cancer diagnosis. CRD42020203990.
Access options
Subscribe to Journal
Get full journal access for 1 year
118,77 €
only 4,95 € per issue
Tax calculation will be finalised during checkout.
Rent or Buy article
Get time limited or full article access on ReadCube.
from$8.99
All prices are NET prices.

Data availability
Data are available upon request to the corresponding author.
References
- 1.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
- 2.
de Sousa Barros AE, Conde CR, Lemos TMR, Kunz JA, da Silva Marques MDL. Feelings experienced by women when receiving the diagnosis of breast cancer. J Nurs UFPE line-Qualis B2. 2018;12:102–11.
- 3.
Mertz BG, Bistrup PE, Johansen C, Dalton SO, Deltour I, Kehlet H, et al. Psychological distress among women with newly diagnosed breast cancer. Eur J Oncol Nurs. 2012;16:439–43.
- 4.
Holland JC, Andersen B, Breitbart WS, Buchmann LO, Compas B, Deshields TL, et al. Distress management. J Natl Compr Cancer Netw. 2013;11:190–209.
- 5.
Drageset S, Lindstrøm TC, Giske T, Underlid K. “The support I need”: Women’s experiences of social support after having received breast cancer diagnosis and awaiting surgery. Cancer Nurs. 2012;35:E39–E47.
- 6.
Epping-Jordan JE, Compas BE, Osowiecki DM, Oppedisano G, Gerhardt C, Primo K, et al. Psychological adjustment in breast cancer: Processes of emotional distress. Health Psychol. 1999;18:315–26.
- 7.
Landmark BT, Wahl A. Living with newly diagnosed breast cancer: a qualitative study of 10 women with newly diagnosed breast cancer. J Adv Nurs. 2002;40:112–21.
- 8.
Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26:768–77.
- 9.
Ridner SH. Psychological distress: concept analysis. J Adv Nurs. 2004;45:536–45.
- 10.
Yang H, Brand JH, Fang F, Chiesa F, Johansson AL, Hall P, et al. Time‐dependent risk of depression, anxiety, and stress‐related disorders in patients with invasive and in situ breast cancer. Int J Cancer. 2017;140:841–52.
- 11.
Lim CC, Devi MK, Ang E. Anxiety in women with breast cancer undergoing treatment: a systematic review. Int J Evid Based Healthc. 2011;9:215–35.
- 12.
Maass SW, Roorda C, Berendsen AJ, Verhaak PF, de Bock GH. The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas. 2015;82:100–8.
- 13.
Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–74.
- 14.
Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–26.
- 15.
Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychol Med. 2010;40:1797–810.
- 16.
Brunet A, Weiss DS, Metzler TJ, Best SR, Neylan TC, Rogers C, et al. The peritraumatic distress inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158:1480–5.
- 17.
Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer: a conceptual and empirical review. Clin Psychol Rev. 2002;22:499–524.
- 18.
Wong M, Looney E, Michaels J, Palesh O, Koopman C. A preliminary study of peritraumatic dissociation, social support, and coping in relation to posttraumatic stress symptoms for a parent’s cancer. Psycho‐Oncol. 2006;15:1093–8.
- 19.
Leano A, Korman MB, Goldberg L, Ellis J. Are we missing PTSD in our patients with cancer? Part I. Can Oncol Nurs J. 2019;29:141–6.
- 20.
Arnaboldi P, Riva S, Crico C, Pravettoni G. A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer (Dove Med Press). 2017;9:473–85.
- 21.
Costanzo ES, Ryff CD, Singer BH. Psychosocial adjustment among cancer survivors: findings from a national survey of health and well-being. Health Psychol. 2009;28:147–56.
- 22.
Ivanauskienė R, Padaiga Ž, Šimoliūnienė R, Smailytė G, Domeikienė A. Well-being of newly diagnosed women with breast cancer: Which factors matter more? Support Care Cancer. 2014;22:519–26.
- 23.
Hanson Frost M, Suman VJ, Rummans TA, Dose AM, Taylor M, Novotny P, et al. Physical, psychological and social well‐being of women with breast cancer: the influence of disease phase. Psycho‐Oncol. 2000;9:221–31.
- 24.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
- 25.
Welch V, Petticrew M, Petkovic J, Moher D, Waters E, White H, et al. Extending the PRISMA statement to equity-focused systematic reviews (PRISMA-E 2012): explanation and elaboration. Int J Equity Health. 2015;14:1–23.
- 26.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9.
- 27.
Linden W, Vodermaier A, MacKenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141:343–51.
- 28.
Kyranou M, Paul SM, Dunn LB, Puntillo K, Aouizerat BE, Abrams G, et al. Differences in depression, anxiety, and quality of life between women with and without breast pain prior to breast cancer surgery. Eur J Oncol Nurs. 2013;17:190–5.
- 29.
Villar RR, Fernández SP, Garea CC, Pillado M, Barreiro VB, Martín CG. Quality of life and anxiety in women with breast cancer before and after treatment. Rev Lat-Am Enferm. 2017;25:1–13.
- 30.
Arnaboldi P, Lucchiari C, Santoro L, Sangalli C, Luini A, Pravettoni G. PTSD symptoms as a consequence of breast cancer diagnosis: clinical implications. SpringerPlus. 2014;3:1–7.
- 31.
Primo K, Compas BE, Oppedisano G, Howell DC, Epping-Jordan JE, Krag DN. Intrusive thoughts and avoidance in breast cancer: Individual differences and association with psychological distress. Psychol Health. 2000;14:1141–53.
- 32.
Tjemsland L, Søreide JA, Malt UF. Traumatic distress symptoms in early breast cancer I: acute response to diagnosis. Psycho‐Oncol. 1996;5:1–8.
- 33.
Holland, JC, Rowland, JH. Handbook of psycho-oncology: psychological care of the patient with cancer. New York: Oxford University Press. 1989.
- 34.
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho‐Oncol. 2001;10:19–28.
- 35.
Montgomery M, McCrone SH. Psychological distress associated with the diagnostic phase for suspected breast cancer: Systematic review. J Adv Nurs. 2010;66:2372–90.
- 36.
Lam WW, Bonanno GA, Mancini AD, Ho S, Chan M, Hung WK, et al. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psycho‐Oncol. 2010;19:1044–51.
- 37.
Witek-Janusek L, Gabram S, Mathews HL. Psychologic stress, reduced NK cell activity, and cytokine dysregulation in women experiencing diagnostic breast biopsy. Psychoneuroendocrinology. 2007;32:22–35.
- 38.
Baqutayan SMS. The effect of anxiety on breast cancer patients. Indian J Psychol Med. 2012;34:119–23.
- 39.
Stark DPH, House A. Anxiety in cancer patients. Br J Cancer. 2000;83:1261–7.
- 40.
Woodward V, Webb C. Women’s anxieties surrounding breast disorders: a systematic review of the literature. J Adv Nurs. 2001;33:29–41.
- 41.
Wu X, Wang J, Cofie R, Kaminga AC, Liu A. Prevalence of posttraumatic stress disorder among breast cancer patients: a meta-analysis. Iran J Public Health. 2016;45:1533–44.
- 42.
Cordova MJ, Riba MB, Spiegel D. Post-traumatic stress disorder and cancer. Lancet Psychiatry. 2017;4:330–8.
- 43.
Kangas M. DSM-5 trauma and stress-related disorders: implications for screening for cancer-related stress. Front Psychiatry. 2013;4:122.
- 44.
Shiban E, Lehmberg J, Hoffmann U, Thiel J, Probst T, Friedl M, et al. Peritraumatic distress fully mediates the relationship between posttraumatic stress symptoms preoperative and three months postoperative in patients undergoing spine surgery. Eur J Psychotraumatol. 2018;9:1423824.
- 45.
Briere J, Dias CP, Semple RJ, Scott C, Bigras N, Godbout N. Acute stress symptoms in seriously injured patients: Precipitating versus cumulative trauma and the contribution of peritraumatic distress. J Trauma Stress. 2017;30:381–8.
- 46.
Cella DF, Cherin EA. Quality of life during and after cancer treatment. Compr Ther 1988;14:69–75.
- 47.
Else-Quest NM, LoConte NK, Schiller JH, Hyde JS. Perceived stigma, self-blame, and adjustment among lung, breast and prostate cancer patients. Psychol Health. 2009;24:949–64.
- 48.
Avis NE, Levine BJ, Case LD, Naftalis EZ, Van Zee KJ. Trajectories of depressive symptoms following breast cancer diagnosis. Cancer Epidemiol Prev Biomark. 2015;24:1789–95.
- 49.
Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, Rafiemanesh H, Hashemi SM, Balouchi A. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. 2019;176:519–33.
- 50.
Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41:2613–9.
- 51.
Brucker PS, Yost K, Cashy J, Webster K, Cella D. General population and cancer patient norms for the functional assessment of cancer therapy-general (FACT-G). Eval Health Prof. 2005;28:192–211.
- 52.
Schnur JB, Montgomery GH, Hallquist MN, Goldfarb AB, Silverstein JH, Weltz CR, et al. Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. Int J Behav Med. 2008;15:21–8.
- 53.
Sohl SJ, Schnur JB, Sucala M, David D, Winkel G, Montgomery GH. Distress and emotional well-being in breast cancer patients prior to radiotherapy: an expectancy-based model. Psychol Health. 2012;27:347–61.
- 54.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51.
- 55.
Tang M, Liu X, Wu Q, Shi Y. The effects of cognitive-behavioral stress management for breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Cancer Nurs. 2020;43:222–37.
- 56.
Song F, Sheldon TA, Sutton AJ, Abrams KR, Jones DR. Methods for exploring heterogeneity in meta-analysis. Ev Health Prof. 2001;24:126–51.
- 57.
Manne S, Kashy D, Albrecht T, Wong YN, Lederman Flamm A, Benson III AB, et al. Attitudinal barriers to participation in oncology clinical trials: factor analysis and correlates of barriers. Eur J Cancer Care. 2015;24:28–38.
- 58.
Civilotti C, Maran DA, Santagata F, Varetto A, Stanizzo MR. The use of the Distress Thermometer and the Hospital Anxiety and Depression Scale for screening of anxiety and depression in Italian women newly diagnosed with breast cancer. Support Care Cancer. 2020;28:4997–5004.
- 59.
Cohen M. Coping and emotional distress in primary and recurrent breast cancer patients. J Clin Psychol Med Settings. 2002;9:245–51.
- 60.
Thomas BC, Pandey M, Ramdas K, Nair MK. Psychological distress in cancer patients: hypothesis of a distress model. Eur J Cancer Prev. 2002;11:179–85.
- 61.
Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:1–8.
- 62.
Bovin MJ, Marx BP. The importance of the peritraumatic experience in defining traumatic stress. Psychol Bull. 2011;137:47.
- 63.
Moher D, Liberati A, Tetzlaff J, Altman DG. & The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
- 64.
Andreu Y, Galdón MJ, Durá E, Martínez P, Pérez S, Murgui S. A longitudinal study of psychosocial distress in breast cancer: Prevalence and risk factors. Psychol Health. 2012;27:72–87.
- 65.
Arnaboldi P, Lucchiari C, Santoro L, Sangalli C, Luini A, Pravettoni G. PTSD symptoms as a consequence of breast cancer diagnosis: clinical implications. SpringerPlus. 2014;3:392.
- 66.
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ. 2005;330:702.
- 67.
Chang HA, Barreto N, Davtyan A, Beier E, Cangin MA, Salman J, et al. Depression predicts longitudinal declines in social support among women with newly diagnosed breast cancer. Psycho‐Oncol. 2019;28:635–42.
- 68.
Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999;22:185–94.
- 69.
Cimprich B, Ronis DL. Attention and symptom distress in women with and without breast cancer. Nurs Res. 2001;50:86–94.
- 70.
Cimprich B, So H, Ronis DL, Trask C. Pre‐treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psycho‐Oncol. 2005;14:70–8.
- 71.
Denieffe S, Cowman S, Gooney M. Symptoms, clusters and quality of life prior to surgery for breast cancer. J Clin Nurs. 2014;23:2491–502.
- 72.
Farragher B. Psychiatric morbidity following the diagnosis and treatment of early breast cancer. Ir J Med Sci. 1998;167:166–9.
- 73.
Faye‐Schjøll HH, Schou-Bredal I. Pessimism predicts anxiety and depression in breast cancer survivors: a 5‐year follow‐up study. Psycho‐Oncol. 2019;28:1314–20.
- 74.
Galloway SK, Baker M, Giglio P, Chin S, Madan A, Malcolm R, et al. Depression and anxiety symptoms relate to distinct components of pain experience among patients with breast cancer. Pain Res Treat. 2012;2012:851276.
- 75.
Gibbons A, Groarke A, Sweeney K. Predicting general and cancer-related distress in women with newly diagnosed breast cancer. BMC Cancer. 2016;16:935–43.
- 76.
Glinder JG, Compas BE. Self-blame attributions in women with newly diagnosed breast cancer: a prospective study of psychological adjustment. Health Psychol. 1999;18:475–81.
- 77.
Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL, et al. Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer. 2006;107:2924–31.
- 78.
Hegel MT, Collins ED, Kearing S, Gillock KL, Moore CP, Ahles TA. Sensitivity and specificity of the distress thermometer for depression in newly diagnosed breast cancer patients. Psycho‐Oncol. 2008;17:556–60.
- 79.
Henselmans I, Helgeson VS, Seltman H, de Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol. 2010;29:160–8.
- 80.
Jones SM, LaCroix AZ, Li W, Zaslavsky O, Wassertheil-Smoller S, Weitlauf J, et al. Depression and quality of life before and after breast cancer diagnosis in older women from the Women’s Health Initiative. J Cancer Surviv: Res Pr. 2015;9:620–9.
- 81.
Kaiser J, Dietrich J, Amiri M, Rüschel I, Akbaba H, Hantke N, et al. Cognitive performance and psychological distress in breast cancer patients at disease onset. Front Psychol. 2019;10:2584.
- 82.
Kant J, Czisch A, Schott S, Siewerdt-Werner D, Birkenfeld F, Keller M. Identifying and predicting distinct distress trajectories following a breast cancer diagnosis-from treatment into early survival. J Psychosom Res. 2018;115:6–13.
- 83.
Kennedy F, Harcourt D, Rumsey N, White P. The psychosocial impact of ductal carcinoma in situ (DCIS): a longitudinal prospective study. Breast. 2010;19:382–7.
- 84.
Lally RM, Bellavia G, Gallo S, Kupzyk K, Helgeson V, Brooks C, et al. Feasibility and acceptance of the caring guidance web‐based, distress self‐management, psychoeducational program initiated within 12 weeks of breast cancer diagnosis. Psycho‐Oncol. 2019;28:888–95.
- 85.
Lee KM, Jung D, Hwang H, Son KL, Kim TY, Im SA, et al. Pre-treatment anxiety is associated with persistent chemotherapy-induced peripheral neuropathy in women treated with neoadjuvant chemotherapy for breast cancer. J Psychosom Res. 2018;108:14–9.
- 86.
Miranda CRR, De Resende CN, Melo CFE, Costa AL, Friedman H. Depression before and after uterine cervix and breast cancer neoadjuvant chemotherapy. Int J Gynecol Cancer. 2002;12:773–6.
- 87.
Ng CG, Mohamed S, Kaur K, Sulaiman AH, Zainal NZ, Taib NA, et al. Perceived distress and its association with depression and anxiety in breast cancer patients. PLoS ONE. 2017;12:e0172975.
- 88.
Oh PJ, Cho JR. Changes in fatigue, psychological distress, and quality of life after chemotherapy in women with breast cancer: a prospective study. Cancer Nurs. 2020;43:E54–E60.
- 89.
Oliveri S, Arnaboldi P, Pizzoli SFM, Faccio F, Giudice AV, Sangalli C, et al. PTSD symptom clusters associated with short-and long-term adjustment in early diagnosed breast cancer patients. Ecancermedicalscience. 2019;13:917.
- 90.
Park EM, Gelber S, Rosenberg SM, Seah DS, Schapira L, Come SE, et al. Anxiety and depression in young women with metastatic breast cancer: a cross-sectional study. Psychosom. 2018;59:251–8.
- 91.
Ramalho M, Fontes F, Ruano L, Pereira S, Lunet N. Cognitive impairment in the first year after breast cancer diagnosis: a prospective cohort study. Breast. 2017;32:173–8.
- 92.
Romeo A, Di Tella M, Ghiggia A, Tesio V, Torta R, Castelli L. Posttraumatic growth in breast cancer survivors: are depressive symptoms really negative predictors? Psychol Trauma: Theory Res Pr Policy. 2020;12:244–50.
- 93.
Stafford L, Judd F, Gibson P, Komiti A, Mann GB, Quinn M. Screening for depression and anxiety in women with breast and gynaecologic cancer: course and prevalence of morbidity over 12 months. Psycho‐Oncol. 2013;22:2071–8.
- 94.
Voigt V, Neufeld F, Kaste J, Bühner M, Sckopke P, Wuerstlein R, et al. Clinically assessed posttraumatic stress in patients with breast cancer during the first year after diagnosis in the prospective, longitudinal, controlled COGNICARES study. Psycho‐Oncol. 2017;26:74–80.
- 95.
Watson M, Greer S, Rowden L, Gorman C, Robertson B, Bliss JM, et al. Relationships between emotional control, adjustment to cancer and depression and anxiety in breast cancer patients. Psychol Med. 1991;21:51–7.
Acknowledgements
The authors thank the members of Dr Brunet’s lab (Research Laboratory on Psychological Trauma) and Dr. Marin’s lab (Stress, Trauma, Emotions, Anxiety and Memory [STEAM] lab) for their generous feedback. The authors are thanking Dr. Bernard Fortin, MD, for providing his expertise in oncology. Dr. Marie-France Marin is thanking the Fonds de Recherche en Santé du Québec for a salary award. Finally, the authors thank Connie Guo for linguistic revisions.
Funding
The authors did not receive funding to conduct the meta-analysis.
Author information
Affiliations
Contributions
JF coordinated the study, carried out all the search and wrote most of the paper. ML assisted JF in all stages of the project, she also reviewed the table of results and wrote some sections of the paper. GE performed the statistical analyses and created the figures and helped with the revisions of the paper. Drs. M-FM and AB provided mentorship at all stages of the study and as the paper was being written and reviewed. Dr. MJC also provided mentorship and precious feedback, especially in the field of breast cancer and mental health. All authors have reviewed this version of the article and agreed to its publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This meta-analysis study did not thus involve human participants, human data or human tissue. No ethics approval or contentment to participate were not required.
Consent to publish
This manuscript does not contain any individual person’s data in any form, thus, consent for publication was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Fortin, J., Leblanc, M., Elgbeili, G. et al. The mental health impacts of receiving a breast cancer diagnosis: A meta-analysis. Br J Cancer (2021). https://ift.tt/38GiIq7
-
Received:
-
Revised:
-
Accepted:
-
Published:
Keywords
- oncology, anxiety
- depression
- psychological distress
- post-traumatic stress
- well-being
"breast" - Google News
September 04, 2021 at 08:23PM
https://ift.tt/3zG6ud3
The mental health impacts of receiving a breast cancer diagnosis: A meta-analysis | British Journal of Cancer - Nature.com
"breast" - Google News
https://ift.tt/2ImtPYC
https://ift.tt/2Wle22m
Bagikan Berita Ini














0 Response to "The mental health impacts of receiving a breast cancer diagnosis: A meta-analysis | British Journal of Cancer - Nature.com"
Post a Comment