“Smarter screening” strategies may play a crucial role in helping Latina and Black women survive breast cancer at the same rates as their White counterparts, according to a presenter at the 5th Annual School of Nursing Oncology virtual conference.
During her presentation, Olufunmilayo I. Olopade, MD, FACP, OON, American Cancer Society clinical research professor at the University of Chicago’s Center for Clinical Cancer Genetics & Global Health, stressed the need to better understand how breast cancer affects Latina and Black women to improve their survival outcomes following treatment.
“We want to make sure we can provide the right treatment for the right patient at the right time,” explained Olopade. “Then, we can keep our families healthy…what we're looking for in preventive oncology, we can do in the clinic and we can also do it in the population. [We] identify individuals who have already had cancer as a way for us to reach their family members.”
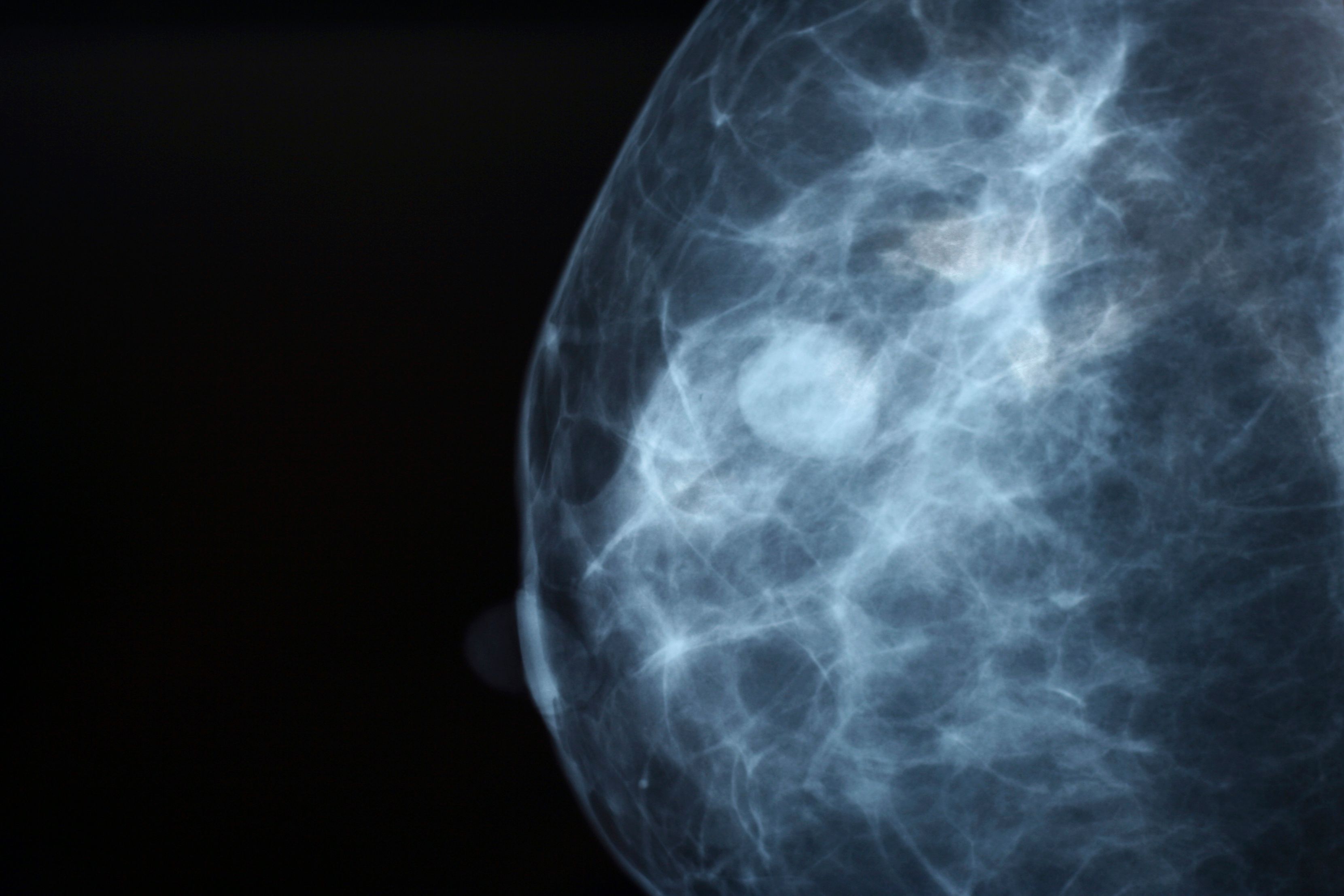
Olopade told the attendees that screening has been an effective tool at reducing breast cancer deaths. However, in her research, Black women in and around the Chicago, Illinois area get screened at rates higher than the national average, yet still have poorer outcomes than White women — even though patients achieve pathologic complete responses at similar rates.
Over time, she said she has learned from genomic assays that breast cancer is not simply one disease but is made up of several different ones. Furthermore, she noted how she has learned that screening for early detection of breast cancer should no longer be age based.
“What we learned from Chicago is that Black and Brown women, and in fact, all young women who get breast cancer under the age of 14, are the ones that are having the worst disparity. In all other cancers, older women tend to do worse,” she said. “We suddenly say, ‘Everyone starts screening at 40,’ [but] there are some women who would have had breast cancer that would have the potential to kill them before they ever get that first mammogram.
“So that’s why we're going away from talking about age-based screening to begin to say, ‘Let us personalize screening.’ Let us all figure out what exactly we are at risk for. Are we at risk for a ‘cheetah’ type of cancer? Or are we at risk for a ‘snail’ type of cancer that grows very slowly?”
Patterns of Inherited Breast Cancer in Black Women
Olopade has studied patterns of inherited breast cancer women in Nigeria, Cameroon, Uganda, Brazil, and among Black women in the United States. Those data, along with findings from the CARRIERS study which included 32,247 women with breast cancer and 32,544 controls, show that BRCA1/2 and PALB2 are the most important genes for assessing breast cancer risk in this patient population. Black women who harbor these genes develop cancer are almost 15 years younger at diagnosis on average compared with White women who carry the same pathogenic variants.1
“These are women who get breast cancer at a very young age. So that’s why we cannot use a one-size-fits-all [approach], and then say, ‘Oh, but you know, BRCA1 and BRCA2 are not important.’ They are important. It all depends on your population. When you test 1000 cases and 1000 controls in Nigeria and you have almost 12% of them showing up with a mutation in BRCA1, BRCA2, or PALB2, you’re going to focus on that as an intervention for cancer control.”
Determining a patient’s individual risk is challenging, in part because Black women tend to be underrepresented in clinical trials in the United States and abroad. Genomic testing for precision risk assessment will transform cancer care, Olopade said.
“We can’t just take what is being shown in White women and then expect it to work for Indian women, expect it to work for Asian women, expect it to work for women from Africa,” she added. “So, what is the heterogeneity? What is it that we need to do for Black and Brown women?”
This is where investigators need to go beyond race and ethnicity, she said. Physicians can use data from genome-wide association studies (GWAS) to develop a polygenic risk score (PRS), which is calculated for an individual based on the presence or absence of risk variants identified in large GWAS studies. PRS can provide better insight than traditional risk models, especially in these populations. The model can estimate risk for a Black or Brown woman based on the proportion of African ancestry in her DNA.
“We can now identify women who are in the top percentile, [representing] 5% of women who have a risk that is actionable before the age of 50. If we can find those women before the age of 50, or even if we can…can really track them [and] counsel them, and then we can put them on a screening, that is going to be different because they are at risk for [estrogen receptor]-negative breast cancer, [and] I think that will really help the field. We’re talking about deescalating—not just using more and more treatment. We have to deescalate in what we're doing for early detection. We have to use innovations.”
References
- Olopade OI. Retooling precision oncology for true equity of cancer care. Presented at: 5th Annual School of Oncology Nursing; August 6-7, 2021; virtual.
- Hu C, Hart SN, Gnanaolivu R, et al. A population-based study of genes previously implicated in breast cancer. N Engl J Med. 2021;384(5):440-451. doi:10.1056/NEJMoa2005936
This article was originally published on OncLive as, “Smarter Screening, Risk Assessments Are Key to Eliminating Racial Disparities in Breast Cancer Outcomes.”
"breast" - Google News
August 11, 2021 at 01:22AM
https://ift.tt/3lSp8dt
Personalized Screenings are Needed to Address Racial Disparities in Breast Cancer Outcomes - www.oncnursingnews.com/
"breast" - Google News
https://ift.tt/2ImtPYC
https://ift.tt/2Wle22m
Bagikan Berita Ini














0 Response to "Personalized Screenings are Needed to Address Racial Disparities in Breast Cancer Outcomes - www.oncnursingnews.com/"
Post a Comment